AN OVERVIEW ON ACUTE EPIGLOTTITIS DIAGNOSIS AND MANAGEMENT IN PRIMARY HEALTH CARE CENTER: A LITERATURE REVIEW
Naif Ali Alamri1*, Mohammed Abdulnasser Alkhateeb 1, Amr Tareq Aboalfaraj1, Asalah Khalid M Alhazmi1, Yasser Abdulrahman Almalki2, Duaa Ahmed Alabbas3, Rihanah Farhan Al-Shahrani4, Hadeel Salem Alwagdani2, Mohammed Muteb Alharbi5, Nadia Anwar Ahmed1, Nuha Hassan Al Subhi6
|
|
|
ABSTRACT
Introduction: Acute epiglottis is a life-threatening condition that can lead to early death if not treated immediately. It is thought that acute epiglottis is a condition that can only affect children; however, adults also can be affected by it. Acute epiglottis can be infectious or non-infectious. The treatment is early intubation for severe cases. Objective: The objective of this review is to discuss acute epiglottis, its clinical and radiological manifestations, and how to deal with it to save the patient’s life. Method: We searched the PubMed database looking for articles relevant to the topic using Mesh terms, "Acute Epiglottis”. Conclusion: Proper history taking, and examination, and radiological study can protect patients from possible loss of their lives since it is an acute life-threatening condition that can lead to rapid deterioration of the patient’s life.
Keywords: Acute epiglottis, Upper Air Ways Obstruction, Haemophilus Influenzae, Endo-Tracheal Intubation.
Introduction
Earlier in the days before discovering the vaccine for Haemophilus Influenzae, acute epiglottis was seen more often in the youngsters aged between 3-5 years [1]. In contrast, nowadays, the acute epiglottis is more commonly happening among adults [1]. These days the causative microorganism is group A β-hemolytic Streptococci instead of the previous Haemophilus Influenzae type b (Hib) [1]. Acute epiglottitis is a potentially fatal condition with serious consequences. It is an anesthesiologist’s nightmare because s/he considers the possibility of a laryngospasm and the permanent loss of the airway [2].
Other noninfectious justifications for acute epiglottitis include trauma, comorbid systemic diseases, and chemotherapy [1]. The familiar microorganisms of acute epiglottitis in adults are Streptococcus pneumoniae, Staphylococcus aureus, and Klebsiella pneumoniae [3].
Pathophysiology:
Acute epiglottis is a sensitive inflammatory condition that is confined to the supraglottic structures that include epiglottis, aryepiglottic folds, arytenoids [2]. It is a serious life-threatening disorder because it may cause marked edema of the epiglottic structures and ultimate blocks or obstructs the airway [2]. It often comes in a sudden nature of onset with children. This makes them at higher risks of airway obstruction [2]. Unlikely, in adults where it frequently comes with other comorbids it doesn’t really give the sings of airway blockage [1].
In children, the responsible causative microorganism is Haemophilus influenzae type b. On the other hand in adults, they are Klebsiella pneumoniae, Streptococcus pneumoniae, and Staphylococcus aureus [4]. In adults, it is better-called supraglottitis instead of inflammation because it usually affects the anatomy adjacent to the supraglottis [4]. These structures involve the pharynx, pseudo-vocal cords, uvula, aryepiglottic folds, and base of the tongue [5].
However, in young adults, inhalation of heated objects when smoking illicit drugs is believed to be sometimes the cause of acute epiglottitis [6]. The symptoms, signs, X-ray, and laryngoscopic findings are pretty similar to those of infectious epiglottitis [2]. These adolescents show a lot of the characteristics observed in acute infectious epiglottitis and should be managed with the same thought for possible upper airway obstruction [2].
Clinical Manifestations and Differential Diagnosis:
Acute epiglottis can still happen in children due to the failure of immunization or other causative pathogens [1]. Since it is an emergency, it is important to differentiate acute epiglottitis from other medical conditions as it may cause serious airway obstruction, specifically croup [7]. There are key differentials to bear in mind when looking into both conditions [7]. For example, both can come with pyrexia, stridor, and shortness of breath. Yet, acute epiglottitis comes with generalized toxemia, severe soreness of the throat, and extreme pain or difficulty swallowing [7]. This inability to swallow causes the patient to drool [8]. Hence, it is a very important differentiating sign of epiglottitis. Here the patient will be situated in the “tripod position", which is having him or her sit up and lean forward as if the patient is sniffing while breathing through the mouth opened and the tongue protruded [9]. Where the croup has coughing but not drooling [7]. To sum it up, in children the most frequent signs are muffled voices, drooling, dyspnea, and inspiratory stridor if present [1].
Foreign body and croup in the upper airway are the most common differential diagnosis. The differentiation between acute epiglottitis with its serious consequences and less urgent causes of a sore throat, shortness of breath, and dysphagia may become difficult due to the late referral to an acute care center [2]. Antibiotic therapy is administered regardless of bacterial culture, with the consequence of negative cultures at admission [2]. The most common etiology of croup is viral laryngotracheobronchitis, which results in swelling of the mucosa in the subglottic area of the larynx [10]. Chart 1 explains the differences and similarities of acute epiglottitis and croup.
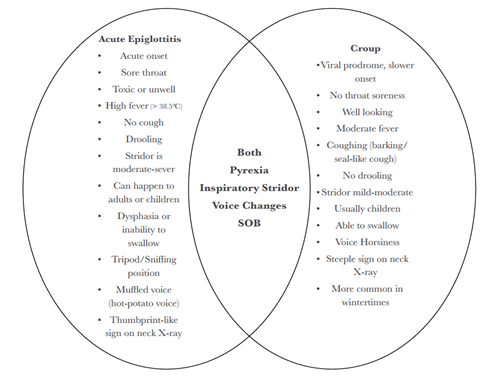
Chart 1: Acute Epiglottis vs Croup
Whilst in adults, the presentation is a bit different. In adults, symptoms are discomfort upon swallowing besides the severe pain and distinguished voice changes due to the inflammation of the pharynx [4]. These can accompany pyrexia, toxemia, cervical lymphadenopathy, and cellulitis on the chest and neck [11]. Additionally, it can be preceded by upper respiratory tract infection (URTI) symptoms. Ages that are involved in experiencing acute epiglottitis are between 42 to 48 years having more males than females to the ratio of 2.5:1, respectively [11].
Diagnosis:
To diagnose acute epiglottitis in children, physicians have to be extra cautious. That is because they might induce airway obstruction [2]. Best care for such a situation is to be in the operation room with anesthesiologists and otolaryngologists [2]. Imaging is the mainstay for diagnosing acute epiglottitis in children [12]. A common finding on a classical neck radiograph would be a “thumbprint-like” epiglottis which is enlarged with aryepiglottic folds that are edematous [12].
In adults, it is more appropriately called supraglottitis and physicians can be more comfortable when doing extra workups. Like neck x-rays from the lateral aspect, a typical sign would be the thumbprint sign of the epiglottis, a gross epiglottic shadow as it is swollen, and the effacement of the vallecula which makes the known “vallecula sign”[13]. Clinical symptoms and signs remain more important as the imaging of soft tissue can be misleading. Other workups can be ultrasonography and laryngoscopy [2, 14]. Precipitation of airway obstruction in adults is not caused by the indirect, direct, and flexible laryngoscopes as they are even more accurate and airway friendly [1]. However, ultrasonography has been identified as a way to examine the epiglottis [14].
Treatment:
In the past, tracheostomy was the mainstay for the treatment of acute epiglottitis [15]. Yet, currently, general anesthesia and endotracheal tubes are the standard management [1]. Patients who are having signs of progressive upper airway obstruction, homogenous with acute epiglottitis, should be treated as both a medical and an airway emergency [1]. The patient will start with immediate airway, breathing, and circulation with a high flow of oxygen and intravenous access [16]. Analysis of arterial blood gas, full blood count, and blood cultures help to take decisions towards the requirement for intubation and the following treatment, but they are not often helpful to confirm the diagnosis immediately [16]. Securing the airway must be prioritized over diagnostic procedures and radiography in the presence of respiratory distress [2]. Tracheal intubation is regarded as a potentially difficult procedure of a patient with epiglottitis [2]. The procedure of intubation should be done in precise secure conditions, which is in the operating room, while spontaneous ventilation shall be maintained [16]. The promptness of a team competition in carrying out an immediate tracheotomy should be confirmed [16]. Then the patient should be shifted to the operating room under the charge of an experienced anesthesiologist and surgeon [16]. Especially in children, the induction may be excused with the patient sitting upright [16]. Forcing the child or patient to be in a supine position may result in acute airway obstruction [16]. The method of choice has been described as anesthesia induction with achievement of a deep level of anesthesia and maintenance of spontaneous ventilation [16]. Considering the airway obstruction, the amount of time necessary to produce deep anesthesia using an inhalation induction may be increased secondarily and may necessitate increasing gas concentration, too. In order to determine the anesthetic depth capnography with exhaled gas analysis is useful. Muscle relaxants should not be administered as well as maintaining a spontaneous ventilation is important [16].
In case of diagnosis of acute epiglottitis, a fiberoptic nasal intubation or rigid bronchoscopy using an endotracheal tube with substantially reduced diameter is preferred [14]. After sedation, the patient shall be transferred to an intensive care unit (ICU) after securing the airway. The intravenous sedation should preferably allow voluntary ventilation [14].
Tracheal extubation must be preceded by a cuff leak test with a deflated cuff and, usually, a second look by direct laryngoscopy with deep sedation or general anesthesia [17].
In trying to limit pharyngeal edema and thereby reducing the obstruction of the airway, dexamethasone treatment or budesonide aerosols can be used. The use of corticosteroids has been associated with shorter ICU and overall length of stay, with an average overall length of stay of 3.8 days in adults [11]. Generally, therapies such as sedation, inhalers, or racemic epinephrine should be avoided. Administration of supplemental humidified oxygen should be established if possible, but the patient should not be forced, as this may agitate the illness then could worsen the condition [16].
Prognosis and Complications:
With appropriate and timely treatment, the prognosis in adults with acute epiglottitis is good [12]. However, missed acute epiglottitis may rapidly lead to airway obstruction and results in death [2]. That is because of the sudden airway obstruction and difficulty in intubating those who are affected due to the extensive swelling of supraglottic structures [2]. Acute epiglottitis may cause absolute blockage of the airway and then ultimately death [2]. Even under the best care, complications may still happen, especially in those patients who are immunocompromised [1]. They are at higher risks of complications such as epiglottic abscesses, descending necrotizing mediastinitis, reoccurrence of diseases, and granuloma of vocal cords [6]. The epiglottic abscess shall be drained plus administration of antibiotics intravenously [1].
Conclusion:
Physicians should have a solid background about the basic concept of the clinical presentation, most important workups, and treatment plan of a patient with acute epiglottitis, especially those who are at the emergency department. There shall be a team of anesthesiologists and otolaryngologists involved for the best outcomes and ease of managing successful intubation of the patient’s airway. Acute epiglottitis is an infectious life-threatening condition, which needs to be diagnosed as early as possible and be treated promptly to avoid serious complications, like airway obstruction the asphyxia (death). The establishment of the flexible fiberoptic nasopharyngolaryngoscopy makes seeing the larynx and assessing other possibilities of the compromised airway a more precise function than to just depend on the sometimes faulty soft tissue imaging from the lateral X-rays of the patient’s neck. In a child, the typical presentation of epiglottitis includes acute onset of high temperature, inspiratory stridor, and drooling. Nevertheless, adults may present with supraglottitis, which is the inflammation of the supraglottic larynx and surrounding pharyngeal structures, with predisposing symptoms of pain upon swallowing, dysphagia, and voice changes out of proportion to the inflammation of the pharynx. Lateral neck radiographs with the thumbprint (Figure 1) or vallecula sign can help in confirming the diagnosis of acute epiglottitis if the patient’s airway is stable. Importantly, in a child with epiglottitis and airway that are compromised, physicians should exclude laryngoscopy until the airway is secured in the operating room. Adults are more likely to bear invasive diagnostic procedures, such as flexible fiberoptic laryngoscopy without compromising the airway. All case scenarios need physicians to own a high index of suspicion and promptly establish a treatment to appropriately manage children and adults who are presenting with acute epiglottitis or supraglottitis.

Figure 1: The Thumbprint Sign in Lateral X-Ray.
References
