CHARACTERISTICS OF NEUROLOGICAL MANIFESTATIONS IN HEMATOLOGIC MALIGNANCY PATIENTS AT SAUDI UNIVERSITY HOSPITAL
Aysha A. Alshareef
|
|
Department of Internal Medicine, Neurology Unit, Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia. |
ABSTRACT
Background: Malignancies often affect the nervous system and causes considerable neurologic morbidity and mortality. These effects may directly involve the brain, spine, or peripheral nervous system (PNS) or indirectly affect the nervous system such as paraneoplastic neurologic syndromes. Objective: This study aimed to detect the prevalence of neurological manifestation among hematologic malignancies patients in relation to their treatments’ outcomes. Subjects and methods: This retrospective medical record-based study was performed on all patients with hematologic malignancies who were admitted to King Abdulaziz University Hospital from 2009-2016. Results: Out of 138 (36.9%) patients with hematologic malignancy showed neurological manifestation after radiotherapy or chemotherapy. The most common neurological manifestations were headache (13.6%), dizziness (8.3%) and back pain (7.8%). Death occurred in 21.2% of patients with neurological manifestations versus 13.9% in patients without neurological manifestations. The mortality rate in patients with headache, change in cognition, limb thickness and stroke were 38.5, 38.5, 26.9 and 23.1% respectively. The mortality rate was significant higher (p<0.001) among older patient than others. Conclusion: this study threw the light on the prevalence of neurological manifestations in patients with hematologic malignancies. this is important for the neurologists as well as hematologists and anyone involved in treating patients with hematologic malignancies to be aware of such neurological manifestation and how to diagnose and treated it in order to help provide a better quality of life for those patients.
Keywords: Headache, Metastasis, Hematologic, Cancer, Death, Prevalence, Para-neoplastic syndrome
Introduction
Cancer, in general, is considered one of the leading causes of death worldwide. Neurologic manifestations of recurrent cancer are considered frequent and reported to be accompanied by higher rates of morbidity and mortality [1]. Neurological complications cancer that arises outside of the nervous system can often cause distress, disability, and can be fatal. Neurologic problems are considered the most common reason for hospitalization in patients with systemic cancer other than routine chemotherapy. These neurological complications are presented with similar signs and symptoms associated with various neurological disorders which make it difficult to be easily diagnosed. Comorbid neurological illnesses are commonly presented in old patients with cancer which also adds to the difficult diagnosis [2, 3].
These neurological complications are diverse and can affect any level of the central and peripheral nervous system. The most common tumors known to induce these complications are those coming from the lung, breast, colon, rectum, prostate gland, head, and neck, as well as tumors related to leukemia and lymphoma [4]. In a more recent study, hematologic malignancies have been reported to the second most common neoplasm to be associated with neurological manifestations after breast cancer [1].
Direct affection to the nervous system includes brain metastases, epidural spinal cord compression, leptomeningeal metastases as well as cranial or peripheral various neuropathies. Vascular and metabolic abnormalities, infections and para-neoplastic syndromes were among the common indirect effects of systemic cancer on the nervous system [2]. Recently, neuromuscular disease, including neuropathy, has been described as the most frequent, neoplasm-associated with neurological manifestations followed by central nervous system metastasis, primary headaches, seizures and stroke [1].
The central nervous system and the peripheral nervous system may be involved in the neurologic complications of cancer. These complications can occur as metastasis in different areas like brain, leptomeninges, plexus and skull base. Apart from brain metastasis, the neurologic complications affecting these other sites are not frequent. Overall, they affect about 25% of patients with metastatic cancer and lead to significant morbidity and mortality [5].
To our knowledge, no previous studies have investigated the prevalence of neurological manifestations in patients with hematologic malignancies in specific. Therefore, this study aimed to describe the neurological manifestations among Saudi patients with hematologic malignancies and to identify the prevalence and its impact on patient outcomes.
Subjects and Methods
This retrospective medical record-based study was reviewed and approved by the biomedical research ethics committee at the Faculty of Medicine, King Abdulaziz University (KAU), Jeddah, Saudi Arabia. It was conducted at KAU Hospital (KAUH), Jeddah, Saudi Arabia, and included all patients with hematological malignancies admitted and treated to KAUH between 2009 and 2016 while other oncology patients were not included.
A data collection sheet was designed to collect three types of data that included study variables. These included socio-demographic data (age, gender, nationality, and marital status), medical characteristics (oncological diagnosis, radiological investigation, therapy advised, and neurological manifestations) and outcomes (improved, cured, dead). Dependent study variables included neurological manifestations while independent variables included age, gender, marital status, and oncological diagnosis.
Statistical analysis
Data were collected and entered into the computer. They were analyzed using SPSS version 21. Classification data are presented as numbers and percentages, while numerical data are presented as median (quartile). Chi-squared (χ2) test was applied to detect the relationship between aging and death rate. P-values less than 0.05 were considered statistically significant.
Results
Among 374 patients with hematological malignancies who enrolled in this study, about 60% were less than 40 years and about 21% between 41-60 years old. The median age was 30.5 years (Table 1). About 63% of patients and hematological malignancies present in this study had not neurological manifestation, while about 37%of patients had neurological manifestation after radiotherapy or chemotherapy. Among these include headache (13.6%), dizziness (8.3%), back pain (7.8%), neck pain (5.9%) and many other complications (Table 1).
Table (2) shows the outcome of the patient with hematologic malignancies with or without neurological manifestations. It was observed that (27%) patients with neurologic manifestations were improvement versus (13.5%) patients without neurologic manifestation. The percentage of cured patients with neurological manifestations was about 37% versus 44.5% in patients without neurological manifestations. About 21% and 16% of patients with or without neurological manifestation died respectively (Table 2, Figure 1).
The duration of death and onset of neurological insult was less than one year about 20% of patients with neurological manifestations versus about 12% of patients without neurological manifestations. On the other hand, this duration was more than one year approximately 2.5% in patients with neurological manifestations versus about 1% in patients without neurological manifestations (Table 3).
Table 1: Neurological complications of Age and frequency in the case studied
|
Variables |
Number |
% |
|
Age category |
||
|
40 and less |
221 |
59.1 |
|
41-60 |
80 |
21.4 |
|
61-70 |
45 |
12.0 |
|
71 and above |
26 |
7.0 |
|
Unknown |
2 |
0.5 |
|
Number of complications |
||
|
No neurological complication |
236 |
63.1 |
|
One |
68 |
18.2 |
|
Two |
38 |
10.2 |
|
Three |
12 |
3.2 |
|
Four |
9 |
2.4 |
|
Five |
3 |
0.8 |
|
Six or more |
8 |
2.1 |
|
Type of complication |
||
|
Headache |
51 |
13.6 |
|
Dizziness |
31 |
8.3 |
|
Back Pain |
29 |
7.8 |
|
Neck Pain |
22 |
5.9 |
|
Limb weakness |
21 |
5.6 |
|
Altered cognition |
19 |
5.1 |
|
Stroke |
16 |
4.3 |
|
Metastasis |
16 |
4.3 |
|
Disturbance of vision |
13 |
3.5 |
|
Seizure |
12 |
3.2 |
|
Infection |
12 |
3.2 |
|
Swallowing disturbance |
8 |
2.1 |
|
Loss sensation |
6 |
1.6 |
|
Disturbance of sphincter |
6 |
1.6 |
|
Peripheral Neuropathy |
6 |
1.6 |
|
Faints |
5 |
1.3 |
|
Vertigo |
4 |
1.1 |
|
Speech |
4 |
1.1 |
|
Leptomeningeal |
3 |
0.8 |
|
Paraneoplastic syndrom |
2 |
0.5 |
|
Tremor |
1 |
0.3 |
Table 2: Outcome of the patient with hematologic malignancies with or without neurological manifestations
|
Variables |
The outcome of malignancy (in patients with neurological manifestation) |
The outcome of malignancy (in patients without neurological manifestation) |
Total |
|||
|
Number |
% |
Number |
% |
Number |
% |
|
|
Improved |
33 |
27 |
34 |
13.5 |
67 |
17.9 |
|
Cured |
51 |
36.9 |
112 |
44.5 |
163 |
43.6 |
|
Death |
26 |
21.3 |
35 |
13.9 |
61 |
16.3 |
According to the prevalence of mortality among 138 patients with neurological manifestations according to the complication, it was noticed headache and altered cognition were linked with the highest mortality rate (38.5%) followed by limb weakness (about 27%) and stroke. It was noticed that para-neoplastic syndrome, faints, tremors, speech, vertigo were found not to be associated with deaths (Table 4). There was a significant difference in mortality rate among different age groups of patients with hematological malignancies in this study, where the death rate was significantly higher (p<0.001) among older patients than other patients (Figure 2).
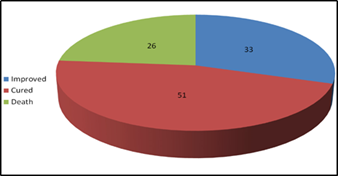
Figure 1: Outcome of a patient with hematological malignancies
Table 3: Duration of onset of neurological insult and death
|
Variables |
Duration in patients with neurological manifestations |
Duration in patients without neurological manifestations |
Total |
|||
|
N |
% |
N |
% |
N |
% |
|
|
More than 1 year |
3 |
2.5 |
1 |
0.4 |
4 |
1.1 |
|
Less than 1 year |
24 |
19.7 |
20 |
7.9 |
44 |
11.8 |
Table 4: Mortality rate in patients with neurological complications
|
Variables |
Number |
% |
|
Headache |
10 |
38.5% |
|
Altered cognition |
10 |
38.5% |
|
Limb weakness |
7 |
26.9% |
|
Stroke |
6 |
23.1% |
|
Dizziness |
5 |
19.2% |
|
Back Pain |
4 |
15.4% |
|
Seizure |
3 |
11.5% |
|
Disturbance of vision |
3 |
11.5% |
|
Infection |
3 |
11.5% |
|
Metastasis |
3 |
11.5% |
|
Leptomeningeal |
2 |
7.7% |
|
Disturbance of sphincter |
2 |
7.7% |
|
Loss sensation |
1 |
3.8% |
|
Neck Pain |
1 |
3.8% |
|
Peripheral Neuropathy |
1 |
3.8% |
|
Swallowing disturbance |
1 |
3.8% |
|
Para neoplastic syndrome |
0 |
0.0% |
|
Faints |
0 |
0.0% |
|
Tremor |
0 |
0.0% |
|
Speech |
0 |
0.0% |
|
Vertigo |
0 |
0.0% |
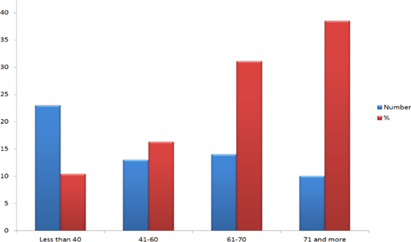
Figure 2: Relationship between age and mortality rate in the studied patients
Discussion
Malignancy often affects the nervous system and cause significant neurologic morbidity and mortality. These effects can be direct which involve the brain, spine, or peripheral nervous system (PNS) or indirectly, such as paraneoplastic neurologic syndromes. In addition, Chemotherapy and radiotherapy can harm the nervous system. This study aimed to calculate the prevalence of neurological manifestation in patients with hematological malignancies admitted to KAUH with cancer with the outcome after treatment.
In this study, approximately 37% of patients with hematological malignancies presented with neurological manifestation after radiotherapy or chemotherapy versus 63% who did not show such manifestations. This is considered a relatively high percentage compared to those previously reported by Newton [2]. He found that 15 to 20 percent of cancer patients have symptomatic neurologic complications during their illness. This percentage increase may be attributed to improved cancer treatments and longer survival in more patients.
In this study, elderly patients between the ages of 61 and 70 years were 12% (n=45) and those older than 70 years represented 7.0% (n=26), while those younger than 40 years accounted for about 60% (n=221) of the patients with hematologic malignancies. Cacho-Díaz et al. reported that 27% (n = 811) of patients with neuro-oncologic consultations were ≥ 65 years of age [6]. This may explain why a large percentage of patients did not have neurological manifestations.
The most common neurological manifestations reported by the patient involved in this study were headache (13.6%), dizziness (8.3%), back pain (about 8%), neck pain (about 6%) and limb weakness (5.6%). Although the same complaints were previously reported by patients with systemic cancer, back pain was ranked first followed by mental status changes, headache, limb pain and leg weakness [2].
In this study, Stroke occurred, in 4.3 % of patients with hematologic malignancies and accounted for approximately 23% of deaths. Stroke has been reported by Dardiotis et al. to be a serious and not a rare complication of malignancy [7]. They added that cancer may directly facilitate stroke occurrence or through cancer-induced hypercoagulation and infections. Cancer treatment options, such as chemotherapy, radiotherapy, and surgery have been described to exacerbate the risk of stroke.
Altered cognition is among relatively common neurological complications detected in about 5% of patients' study, and the mortality rate in such patients with altered cognition was 38.5%. Although the incidence of cancer- and treatment-related cognitive impairment showed great differences in the literature, this rate was ranged from 75% for patients with cancer outside the central nervous system [8] and 90% for CNS cancers [9]. About 25% subset of the cancer survivors may continue to suffer from cognition impairment for a long time after completing their cancer therapy [10]. Some of those cancer survivors reported that cognitive impairment harmed their social and professional lives, and in some conditions [11].
Metastatic complications of the CNS and PNS are relatively rare, but collectively they affect about 25% of all cancer patients [5]. Concerning neuronal metastases, is present while at least half of patients have brain metastases followed by leptomeningeal metastases (LM) [12]. The most common presenting symptoms of LM are pain, sensory changes, and weakness [13]. These findings were in partial agreement with our study because of the frequent neurological manifestation pain reported by patients with hematologic malignancies in this study. The reported forms of pain included headache (13.6%), back pain (about 8%), neck pain (about 6%) and limb weakness (5.6%). On the other hand, the study reported less sensation (1.6%) and disturbance of sphincter (1.6%) by patients. This finding contradicts Schiff and O'Neill who reported that bladder and bowel dysfunction were reported to be a late complication while many recent studies have shown that more than half of patients with cancer presented with bladder/bowel dysfunction [13].
In this study, seizure (3.5%) and visual disturbance (3.5%) were reported by a significantly low percentage of patients, while they were reported to be frequently seen in cancer patients with neurological presentations and were attributed to intracranial dural metastases [14].
In this study, the mortality rate was (21.3%) in patients with neurological manifestation versus(13.9%) in patients without neurological manifestation. Gilbert & Grossman reported that neurologic complications indicate that a significant cause of disability is worse prognosis during the clinical course of the disease; in many cancer centers, neurological problems are the main reason for unplanned hospital admission [15].
Among the limitations of the study were missing data and limited study time.
Conclusion
This study showed the prevalence of neurological manifestations in patients with hematologic malignancies. It is important that neurologists, as well as hematologists and anyone involved in treating patients with hematologic malignancies, be aware of such neurological manifestation and how they are diagnosed and treated so they can help to provide a better quality of life for those patients.
Acknowledgment
The author would like to thank Laila Almalki, Yasmin Sharton, Abdulaziz Aljohani, Firas Alghaffari, Ahad Alsawat, the Medical students of the Faculty of Medicine, KAUH, Jeddah, SA for their help in data collection.
Conflict of interest
The author has no conflict of interest.
References
