AN OVERVIEW OF HIP FRACTURE EVALUATION & MANAGEMENT APPROACH: LITERATURE REVIEW
Fahad Abdulmohsen Almejrad1, Abdulrahman Fayez Shubat Alotaibi2, Maisa Mubarak A Albarakati3, Abdullah Ahmed Sufyani4, Arwa Modawi Asiri5, Abdulrahman Anis Khan6, Abdullah Mohammed A Asiri5, Ali Hussain Ali Al-Shuhayb7, Mohammed Munir Alshahrani5, Mazen Abdullah Mohammed5*, Saad Ali Alwadai5
|
|
|
ABSTRACT
Background: The hip joint is a ball-and-socket joint composed of the acetabulum and head of the femur. The hip is like any other bony structure and is prone to fractures, those can be classified as either intracapsular or extracapsular injuries. Elderly patients form the majority of hip fracture cases, especially women. Studies suggest an increase in hip fracture incidence as the life expectancy of the population increased as well. Surgeons, practitioners, and caregivers equally are obligated to be aware of the presentation and risk factors to guarantee early detection of the problem and avoid possible fatal complications. Objectives: We aimed to review the literature reviewing hip fractures, risk factors, clinical presentation, diagnosis, and management of this injury. Methodology: We used the PubMed database to select relevant articles, chosen papers had undergone an in-depth review. Conclusion: The tailored management plan, whether surgical or conservative, must be selected carefully taking into consideration each patient’s specific needs and comorbidities. Options range from weight-bearing training, braces, to closed and open reduction and fixation. In some cases, a partial or a total hip joint replacement is indicated if the patient condition and status permit.
Keywords: Hip fractures, Diagnosis, Management, Types of hip fracture, Hip arthroplasty
Introduction
The hip joint is one out of two ball-and-socket joints in the body, along with the shoulder joint. The anatomy of the hip joint consists of the acetabulum (socket) and the head of the femur (ball) [1-4]. Both are adequately seated in place by thick capsules and strong ligaments, namely pubofemoral, the iliofemoral, ischiofemoral ligaments, and pubofemoral. The incidence of hip fracture has been increasing recently, as the life expectancy of the world population increased as well. A paper suggested that by 2050, 6.26 million hip fractures will occur yearly, those calculations were estimated based on a study in 1990 which found an incidence of 1.66 million cases at the time. [5] With such anticipation, high demand for care, and prevention of such an injury is expected as well. Hence, this paper aims to provide an update regarding hip fracture’s risk factors, diagnosis, and management.
Methodology
Through PubMed database, the selection process took place to identify the relevant articles, and the following keywords were used in the mesh ((“Hip fracture"[Mesh]) AND (“Diagnosis"[Mesh] OR "Management"[Mesh] OR "Risk factors"[Mesh])). The inclusion criteria are based on including one of the following phrases: Hip fracture, femur neck fracture, risk factors, evaluation, management, and diagnosis. Exclusion criteria were all other articles that did not meet the inclusion criteria; not having any of the inclusion criteria topics.
Review:
Hip fractures can be classified broadly into intracapsular, confined within the acetabulum space, and extracapsular. Intracapsular, as its name indicates, includes femoral head and neck, whereas extracapsular includes trochanteric (lesser and greater), intertrochanteric, and subtrochanteric. Figure 1 shows an illustration of different types of fractions.
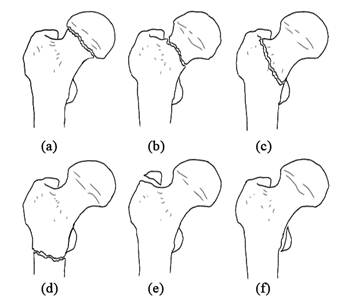
Figure 1: explains the different sites of hip joint fracture, intracapsular: subcapital neck fracture (a) and transcervical neck fracture (b). Extracapsular: intertrochanteric fracture (c), subtrochanteric fracture (d) fracture of the greater trochanter (e), and fracture of the lesser trochanter (f).
Risk Factors
Multiple factors contribute to the probability of fracturing the hip, those can be further categorized into modifiable and non-modifiable factors. Being a woman, by default, results in a 10% to 15% lifetime risk of developing a hip fracture moreover in both the United States and Europe, some studies suggested an even higher risk of 80%. [6, 7] Another non-modifiable factor is age; the risk steeply goes up as the age advances beyond 65. [8] The first occasion of a hip fracture would not only affect the life quality of the patient but also increase the odds of sustaining a subsequent similar injury. [9] Moreover, a positive family history contributes significantly to overall bone fracture risk. [10] The vicious cycle of modifiable risk factors can be traced back to its origin; vitamin D deficiency. [11] As it plays a major role in the pathophysiology of osteoporosis and osteopenia, consequently the bone fragility would actively increase the overall risk of fractures including the hip. [12, 13] This cycle will continue by limiting the level of activity, which is a significant independent factor of hips fracture. [14] The Elderly often are paired with polypharmacy; multiple drugs are used to treat their multiple chronic diseases that can increase the risk of falls. All of the following have shown an increased associated risk of fractures as well levothyroxine, proton pump inhibitors, and psychoactive medication. [15-18]
Clinical Presentation
In hip fracture cases, the surgeon should be alert to the patient’s background and current status. Taking a proper history is a key factor to identify the possible risk factors, hence understanding the probable other injuries, anticipating the prognosis, and preventing the recurrence if possible. The elderly population tends to acquire the injury out of falls from standing heights, middle-age from elevated heights falls, while younger subjects’ fractures are usually related to road traffic injuries. [19] Elderly stress fractures’ pain can initially be triggered by activity, not responding to over the counter pain killers and persists afterward for the upcoming hours. The pain usually is well-located at the groin region and sometimes can be referred to the distal femur or upper knee. On the other hand, the younger population presents with more severe pain due to the abrupt onset of the fracture and maybe with a shortened limb due to the disturbed anatomy. Other physical examination findings include tenderness upon palpation of the groin area and pain with both passive and active movement of the hip joint. The competent surgeon must pay sufficient time to check on the peripheral circulation and use a doppler if indicated.
Diagnostic testing
The initial radiological testing step for all hip fracture cases is a plain X-ray. The preferred positions are anteroposterior (AP) views and cross-table lateral of the pelvis and hip, usually, these capture adequate films to establish the diagnosis. The surgeon should not request the frog-leg view; as it will elicit severe pain and may result in the displacement of the fracture. [20] If the fracture did not appear in the X-ray and the clinical findings consisted of the diagnosis, magnetic resonance imaging (MRI) or a bone scan can be used in such cases. Moreover, in these “occult” fractures magnetic resonance imaging is the gold standard. [21] Aside from the specific testing for the patient, routine laboratory testing and electrocardiography should be obtained as the patient management plan mostly rely on surgical intervention.
Management
The primary assessment of the patient's general condition determines the suitable action plan for each individual. Severe comorbidities hinder proceeding with the surgical option; as it may lead to even worse complications. Bleeding risk, for instance, can be predicted by the presence of two of the following: initial hemoglobin level <12 g/dL, age ≥75 years, and peri-trochanteric fracture. [22] For this group of patients, physiotherapy by early mobilization and weight-bearing exercises might be a reasonable alternative to surgery. [23] If the surgery is the way to go, the choice between general and regional anesthesia should be made. Despite the general anesthesia is the common practice in hip surgery, a recent meta-analysis suggested that neuraxial anesthesia resulted in reduced hospitalization time and in-hospital mortality. [24] Timing is another crucial factor when it comes to better outcomes, patient who underwent surgery within 24 to 48 hours of fracture onset would have early mobilization and rehabilitation. Consequently, obtaining earlier functional recovery would decrease the risk of post-surgical complications, namely pneumonia, deep venous thrombosis, skin lesions, and urinary tract infections. [25] Trochanteric fractures, either greater or lesser, usually present in isolated avulsion fractures form that mainly occur in the younger and active population. [26] Conservative-nonoperative management is the preferred option in these fractures, except for the cases of substantial displacement (≥1 cm), where a reduction might be required. [27] For Intertrochanteric fractures, they may be treated with either arthroplasty or open reduction and internal fixation. [28]
Femoral neck fractures are further classified from I to IV according to Garden’s classification, see Table 1. [29] Nondisplaced fraction usually underwent fixation with preserving of the femoral head while displaced fractures can be treated by reduction and fixation. In displaced neck fracture (Garden’s III-IV) reduction and fixation may result in non-union and avascular necrosis in 30-50% of the patients who underwent this procedure, therefore femoral head replacement is a better choice. Femoral head replacement can be either by replacing the femoral head (hemiarthroplasty), or a total hip replacement, where the femoral head and acetabulum are replaced. [7]
|
Table 1. Garden’s classification for femoral neck fractures |
||
|
Type |
Description |
Displacement level |
|
I |
Valgus impacted incomplete fracture Disruption of the lateral cortex; medial cortex preserved |
Nondisplaced |
|
II |
Complete fracture |
Nondisplaced |
|
III |
Complete fracture Partial displacement |
Displaced |
|
IV |
Complete fracture Complete displacement |
Displaced |
Conclusion
Hip fracture is one of the most disturbing injuries that occurs especially in the elderly population because it hurts their daily life routine. Surgeons must be aware of the patient’s specific situation, history, and type of injury to reach the most efficient management plan with optimum outcomes. Surgical intervention is the mainstay in treating hip fractures with different possible procedures, including, but not limited to, open and closed reduction, fixation, and arthroplasty.
References
