Abstract
The article is devoted to enhancing the effectiveness of the treatment of chronic generalized periodontitis of mild severity, which is an important problem in modern dentistry. According to WHO, periodontitis is the most common therapeutic disease. The purpose of this study was to choose a method for the treatment of chronic generalized periodontitis of mild severity, in which a comparative analysis was performed between the traditional treatment method and the new generation M-chip preparation, which is a nanomatrix based on medical gelatin containing 0.07% miramistine solution. 54 patients participated in the study. According to the results of the study, the treatment of patients with the matrix showed a significant positive effect compared to those in conservative therapy.
Keywords: Chronic generalized periodontitis of mild severity; M-chip; Miramistine
Introduction
According to a number of authors, periodontal diseases, which are a complex multifunctional infections of the structures around the teeth, are one of the key problems of modern dentistry [1, 2]. The greatest risk of periodontal pathology development is determined by the high degree of dental system disorders, the development of purulent diseases of the maxillofacial region, as well as immune system sensitization and chronic intoxication [3, 4]. According to WHO data, every person over 30 years of age suffers from periodontal diseases to some extent [5, 6]. It is known that in the general structure of medical care for patients with dental profile, the patient with periodontal pathology accounts for up to 90% of the total number of meetings in the therapeutic profile [7, 8]. By mediating literary search data, a number of microorganisms, such as Gram-negative anaerobes, play a leading role in the development of the periodontal inflammatory process including Porphyromonas (P. gingivalis, P. melaninogenica), Anaerospirillum, Fusobacteria, Actinomycetes (A. naeslundii, A. viscosus, A. israelii), and streptococcus. Among other listed microorganisms, the most important anaerobic periodontopathogens are A. actinomycetemcomitans, P. gingivalis, and P. intermedia [6, 9, 10]. At present, it can be considered that the quintessence of microbial flora is rightly considered a microbial plaque, leading to infiltration by components of the inflammatory reaction and leading to damage to periodontal tissues with the resulting consequences. As is known, the treatment of periodontal diseases is exclusively individualized, taking into account the universal status [11, 12]. An important role in preventing the development of periodontal diseases is the use of preventive therapy at the stages of Supportive Periodontal Therapy (SPT), as well as oral hygiene, which is a cornerstone in the prevention system, primarily the patient’s awareness of its need [13, 14]. In the absence of proper prevention methods, the need to treat periodontal pathology becomes apparent.
In the methods of treatment, exactly as in the etiopathogenetic cascade of the development of inflammatory periodontal diseases, there is no certain consensus, which determines the polymorphicity of pathology. In this regard, the treatment of periodontal diseases is a set of measures aimed at achieving prolonged remission, according to which the etiotropic approach should be based on complete destruction and elimination of dental plaque [15-17]. The tactics of therapeutic measures carried out in patients suffering from periodontal diseases are the application of general and local therapy methods. Drug therapy is characterized by a number of side effects, including the development of antibiotic resistance, allergic reactions, dysbacteriosis, suppression of the growth of oral comments, which are characterized by less resistance to drugs [18, 19]. At the same time, it is necessary to use new methods of treatment, which offset the listed negative phenomena.
Among such drugs is nanomatrix M-chip. The active ingredient molecule is represented by 0.07% concentration of miramistine based on medical gelatin. A distinctive feature of the "killer" of periodontopathogenic flora is the absence of antibiotics in the composition. Clinical experience of miramistine application, having a wide range of antimicrobial and immunomodulatory action, allows to recommend it for wide application in dentistry, including as a component of drug therapy. Miramistine has a pronounced antimicrobial effect on pathogenic flora including protozoa, fungi, and viruses [20]. The active ingredient molecule dips into the bacterium, breaking the membrane, and changes the permeability of the cell wall at the remaining sites, which determines the antimicrobial effect of the use of this antiseptic preparation [21]. Therefore, there was an interest in following the action of miramistine as an acting agent of nanomatrix in individuals suffering from chronic generalized periodontitis.
The aim of this research was to determine the change of periodontal pocket microflora and reactivity of inflammatory phenomena in patients suffering from chronic generalized periodontitis of mild severity with a background of comparative characteristic of the application of classical treatment technique and use of nanomatrix M-chip.
Research problems
Materials and Methods
In the first stage of the study, based on the analysis of the dental maps of patients of the therapeutic profile, criteria for inclusion and exclusion from the study were determined. The criterion for inclusion in the study was the presence in the patient of a diagnosis of chronic generalized periodontitis K 05.31., which was based on positive basic and additional methods of examination presented by clinical characteristics, dental radiography, and the presence of microbial load. Comorbid status and general disease, the manifestations of which are determined in the oral cavity and burden the course of pathology were a criterion for exclusion from the study.
54 patients were the subject of the study. The treatment was carried out in the therapeutic department of the Dental Polyclinic of GBOU VGO SOGMA of the Ministry of Health of Russia of Vladikavkaz, the Republic of North Ossetia-Alania. Among them, 44 women and 10 men of the IV age group at WHO (35-44 years). Patients were divided into two groups, I-basic (30) and II-control (24) of the corresponding age group. Clinical (X-ray) and microbiological methods were used to examine the patients. A simplified OHI-S oral hygiene index and the level of microbial contamination of periodontal pockets were used to assess the hygienic condition. The anaerobic culture technique involved the isolation of pure cultures on 5% blood heminagar using Himedia anaerostates (UK) and subsequent identification by cultural and biochemical attributes (test system API An, France).
The condition of periodontal tissues was assessed using the PI index, PMA index, SBI hemorrhage index, and periodontal pocket depth measurements.
Basic treatment of patients of the main group (I) was carried out according to the following scheme:
a) General - antibacterial treatment according to antibiotics;
b) Local - irrigation and irrigation of periodontal pockets with 0.01% miramistin solution; Applications of drugs containing anti-inflammatory and antibacterial components;
Basic treatment of group II patients (control) was performed according to the treatment protocol of group I patients, additionally using nanomatrix M-chip. The periodontal pockets, after antiseptic treatment with 0.01% miramistine solution, were dried and the nanomatrix was installed to the full depth of the periodontal pocket locally. After placing the matrix, patients were advised to refrain from eating and drinking for one hour, and not to rinse the oral cavity for 24 hours. Re-installation of the matrix (M-Chip) was carried out in 4 days for 1 month.
The level of hygiene and condition of periodontal tissues in the examined groups was evaluated before treatment and after 14 days, 1 month, and 6 months.
It was found that immediately after the basic treatment, both groups significantly improved the hygienic state of the oral cavity, decreased inflammatory events in periodontal tissues, which was confirmed by positive changes in the indices OHI-S, PMA, bleeding SBI, PI, and the depths of the periodontal pockets and were more pronounced in the main group (I) (Table 1.2). The study of the qualitative composition of the microflora of the periodontal pocket showed that the frequency of release was reduced in the contents of Prevotella intermedia, Peptostreptococcus micros, and Actinomyces israelii. The complete release of the members of periodontopathogenic microflora in most patients did not occur after 6 months.
The results of the study were statistically processed taking into account the representativeness of the Student's criterion, the values of the significant difference were taken as p≤ 0.05.
Results of the research
Table 1: Evaluation of the clinical effectiveness of chronic generalized mild periodontitis in observation dynamics (M±m) (I)
|
Parameters |
OHI-S Hygiene Index, score |
Pi (Pi), score |
PMA % |
Depth of the PK, mm |
Index of gum bleeding frequency,% |
|
Before treatment |
|||||
|
M±m |
1.34±0.11 |
3.52±0.38 |
34.0±2.40 |
3.8±0.2 |
28.6±1.39 |
|
n |
30 |
30 |
30 |
30 |
30 |
|
On the 14th day of treatment |
|||||
|
M±m |
0.2±0.1 |
- |
5.3±0.72 |
did not investigate |
0 |
|
n |
30 |
- |
30 |
- |
0 |
|
31 days after treatment |
|||||
|
M±m |
0.3±0.08 |
1.25±0.13. |
7.4±0.05 |
1.7±0.1 |
0 |
|
n |
30 |
30 |
30 |
30 |
0 |
|
6 months after treatment |
|||||
|
M±m |
0.4±0.1 |
1.42±0.22 |
7.8±0.70 |
1.92±0.2 |
0 |
|
n |
30 |
30 |
30 |
30 |
0 |
Table 2: Evaluation of clinical effectiveness of chronic generalized mild periodontitis in observation dynamics (M±m) (II)
|
Parameters |
OHI-S Hygiene Index, score |
Pi (Pi), score |
PMA % |
Depth of the PK, mm |
Index of gum bleeding frequency,% |
|
Before treatment |
|||||
|
M±m |
1.32±0.15 |
3.21±0.28 |
30.2±3.42 |
3.6±0.2 |
24.7±0.86 |
|
n |
24 |
24 |
24 |
24 |
24 |
|
On the 14th day of treatment |
|||||
|
M±m |
0.8±0.14 |
- |
16.3±2.43 |
не исследовали |
10.0±0.54 |
|
n |
30 |
- |
30 |
- |
0 |
|
31 days after treatment |
|||||
|
M±m |
0.9±0.1 |
2.8±0.20 |
13.6±2.54 |
3.2±0.1 |
15.0 |
|
n |
24 |
24 |
24 |
24 |
3 |
|
6 months after treatment |
|||||
|
M±m |
1.2±0.1 |
3.0±0.24 |
16.5±2.43 |
3.4±0.2 |
15.0 |
|
n |
24 |
24 |
24 |
24 |
3 |
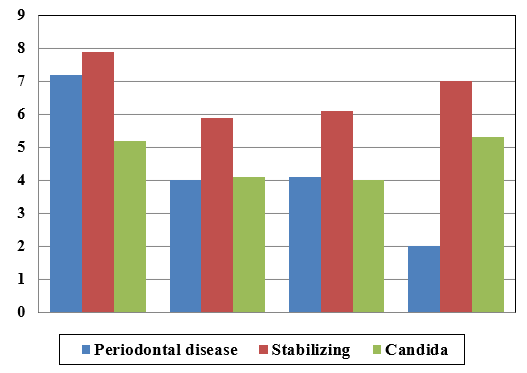
Microbiological evaluation of the effectiveness of local treatment of group I patients (Figure 1) indicated that the contamination of the material of periodontal pockets prior to treatment was extremely high both by members of periodontopathogenic and stabilizing florine-logarithmic microbial number in the range of 7-7.2. There was also high contamination with Candida. On the 14th day of the treatment of patients of the main group, the degree of microbial contamination of periodontopathogenic flora decreased 1.4 times, but the amount of stabilizing flora was normal and remained for the next 6 months.
Figure 1. Dynamics of Microbial Contamination in Comparison to Group I Patients (lg KOE) in Chronic Generalized Mild Periodontitis
Group II patients (Figure 2) showed little progress in reducing the amounts of microflora contained in the periodontal pocket. 1 month after treatment, the microbial number of the periodontal pocket was lg KOE/ml = 6.7, which is 2.5 times higher than in the main group.
Picture 2. Microbial contamination dynamics in group II in comparison to patients in group I (lg KOE) in chronic generalized mild periodontitis
Conclusion
References
