PROPELLER FLAP FOR A SEVERE UNCONVENTIONAL INJURY
Alexandru Adrian1, Oproiu Ana-Maria2, Popescu Ioana3, Dumitrescu Natalia4, Onisâi Minodora5
|
|
|
ABSTRACT
The goal in any reconstruction of soft tissue defects is to restore the function with minimum morbidity and at the same time as esthetic as possible. The lower leg reconstruction algorithm is a subject of debate and the ideal approach has not yet been established. For a long time, the free transfer tissue was the main option. During the last 20 years, with more understanding of local vascularity, the pedicle perforator flaps gained popularity mainly because they have minimal donor-site morbidity, replace the lost tissue with similar tissue coverage and also have a great versatility. We present a case with an unusual mechanism of trauma, a bear bite with a severe avulsion injury cumulated with a high potential for infection, which was reconstructed using a propeller flap.
Keywords: Ankle reconstruction, Propeller flap, Bear bite, Avulsion injury.
Introduction
Treatment of soft-tissue defects on the distal third of the lower extremity is a challenging problem for reconstructive surgeons. [1-3] The difficulty in achieving coverage of such defects is related to the limited amount of muscle and soft tissue around the ankle, the absence of laxity in skin envelope in the lower leg which makes local flaps difficult to design, a suboptimal vascularity with a poor healing capability and with susceptibility to infection, and the presence of weight-bearing forces. [4-8]
The propeller flap is a local island fasciocutaneous flap based on a single dissected perforator and it is designed like a propeller with 2 blades of unequal length with the perforator forming the pivot point, so that, when the blades are switched, the long arm comfortably fills in the defect. [9, 10]
In this paper, we present the use of the propeller flap from the perforators of the peroneal artery in the lower third of the leg. We used this procedure to treat a bear bite, a rarely encountered but severe avulsion mechanism with a great infection potential.
Case History
The patient, aged 40, presented to the Emergency Department after suffering a hunting accident – victim of a bear bite, which resulted in a traumatic amputation affecting the left ankle. The lesion assessment comprised:
• A wound with a diameter of about 10 cm in the left calcaneal region, with highly irregular edges, intensely polluted with foreign bodies (leaves, soil, metal particles).
• Free, torn Achilles tendon, without bone insertion on the heel, with a defect of approximately 6 cm; the patient was unable to perform active dorsiflexion of the foot
• Sensitivity abolished in the left foot
• Lack of bone substance in the calcaneus (calcaneal tuberosity) was detected; the talus was viable.
• Posterior tibial and pedal pulses were present.
In the first stage, we immediately performed surgical debridement of devitalized soft tissue and bony parts, foreign body extraction, abundant lavage, and in collaboration with the orthopedist, heel fixation was practiced with axial Kirschner wires.
The wound was daily cleaned and irrigated. We repeated surgical debridement at day 3 and day 10, and eradicated the obviously nonviable tissue. Negative pressure therapy was also installed, for a total of 7 days starting on day 7.

Fig. 1. A. Clinical and radiological aspect of the wound at the emergency room. B. Clinical aspect after debridement, primary excision of obvious non-viable tissue and skeletal fixation. C. Preoperative and postoperative clinical aspects during the second and third surgical debridement.
Reconstruction was completed on day 14, when the edema decreased, the wound was clean, without any signs of infection, and covered with granulation tissue. We decided to use o propeller flap to cover the soft tissue defect.
Before surgery, we identified 3 perforating vessels with increased vascular signal using a handheld Doppler, located proximally to the defect; they were marked at skin level together with the drawing of the future flap.
Description of the Procedure:
Under general anesthesia, after debridement, we evaluated the soft tissue defect at a dimension of 12/6 cm with bone exposure, absence of calcaneal tuberosity, and defect of Achilles tendon of 4cm (Fig. 2).

Fig. 2. The Final Dimension of the Defect after Complete Debridement of the Necrotic Tissues in the Moment of Reconstruction and the Position of the Distal Perforator Drawn
The skin incision was made in the posterior region according to the preoperative drawing, and the cutaneous perforators were identified by elevation of the lateral margin of the flap at the subfascial level. All the perforators were located according to Doppler examination. The distal septocutaneous perforator, located at 5cm above the lateral malleolus and with 1 mm diameter, was chosen for pivot point of the flap (Fig. 3A).
The distance between the distal perforator and the distal edge of the defect was measured, to ensure that the proximal edge of the flap was reaching the distal margin of the defect without any tension. The flap was elevated as an island fasciocutaneous flap from proximal to distal direction, based on the distal septocutaneous perforator of the peroneal artery (Fig. 3B). The vascular pedicle was prepared and cleared of all muscular and fascial strands, to prevent any compression at this level. After complete dissection of the flap, we verified the perfusion and then rotated 180 degrees the flap in order to reach the heel and cover the defect. The flap dimensions were large (22/7 cm). During the dissection, the small saphenous vein and the sural nerve were cut proximally and distally. As closing materials we used 3/0 monopropylene sutures. Skin grafting was preferred to close the donor defect (Fig. 3).
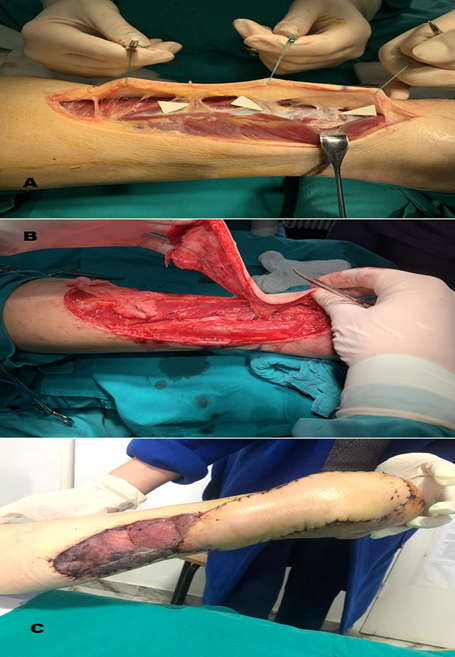
Fig. 3. A. The explorative incision and three perforators of the peroneal artery are identified. B. The flap was risen in subfascial plane and the pedicle was dissected. The recipient site was covered by the major blade of the propeller flap, while the donor area was closed with the small blade and skin graft. C. Fifth day after the reconstruction
Evolution
The postoperative evolution was favorable under antibiotic, anti-inflammatory, anticoagulant and antalgic treatment. The viability of the flap was constantly examined, we observed a normal grade of congestion with normal capillary pulse and without any venous insufficiency. The graft integration percentage to the receptor was 95%, with vascular penetration.
The patient was carefully followed up and a new reevaluation, 14 days later, assessed the pink color of the flap due to neoformation of blood vessels between the receptor bed and the flap, with rapid capillary filling after compression.
We discharged the patient on day 30 after the initial injury, and 2 weeks after the reconstruction, with regular subsequent follow up. No complications were observed and the patient presented a very good general condition.
At 1 year, the evolution is favorable (Fig. 4); the foot dynamic is tolerable to the patient, who refuses ankle arthrodesis.

Fig. 4. The result after 1 year
Discussions
Bear bites are extremely rare and potentially fatal due to the force and ferocity of the attack. Our clinical point of view was to treat the wound like a high energy avulsion injury cumulated with a high potential for infection. Defects resulting from avulsion injuries pose varying degrees of soft tissue and bone loss with uncertain soft-tissue margin viability, greater bony comminution and devascularization. This is bounded by an area with uncertain vascularity with potential for evolution to necrosis and infection, which can further increase the size of the defect.
In the first stage we aimed to obtain a clean defect and to stabilize the ankle. The evidently nonviable soft tissue was surgically debrided and the denuded comminuted bone segments were excised. Also in this stage, the orthopedic surgeon performed fixation of the ankle with two Kirschner wires in order to prevent the movement, and with it, the retraction of the soft tissue.
As the wound needs to be optimized for further intervention, daily bedside debridement and irrigation was applied, in order to provide the most rapid means of cleansing. We repeated surgical debridement on the 3rd day and on the 10th day to eradicate further nonviable tissue. The wound was also treated with negative-pressure therapy, to revitalize the traumatized area - facilitate a better blood supply, decrease the edema and reduce the time to reconstruction. In this phase, our reconstructive options were either muscle flap, local or free transfer, also in order to revitalize the area, or perforating fasciocutaneous flaps, free or pediculated, in case of favorable evolution of the defect. The latter was chosen, as the response to first stage therapy was satisfactory, especially after the negative pressure therapy: limited skin and bone necrosis, wound bed formation of granulation tissue, without any infection and with little edema.
We thus decided to perform an early reconstruction, at about two weeks after the initial injury, with soft tissue reconstruction. When planning any defect reconstruction, we must consider some essential factors such as: defect location, size and requirements, composition defect, general condition of the patient, concomitant injuries, the status of the vascularization of the limb as well as local vascular status, contraindications to certain flaps, surgeon’s familiarity, donor-site morbidity, and patient’s preferences. [11]
Methods of reconstruction for lower limb are locoregional flaps and free transfer tissue. For a long time, free transfer tissue, muscular or fasciocutaneous, was the most frequently performed reconstructive procedure for defects of the distal third of the lower limb due to the paucity of local and regional tissues. During the last decades, the concept of local perforator pedicle based flap has gained increasing popularity based on the growing knowledge and experience with it.
Since their first description in 1989 by Koshima and Soeda [12], perforator flaps opened new perspectives in reconstructive surgery that have reached two important desiderata: muscle preservation and donor site morbidity reduction. Further evolution of perforator flaps has led to the propeller flaps concept which was introduced in 1991 by Hyakusoku and colleagues [13], with later modifications by Hallock [14] and Teo. [9, 15]
The propeller flap is a local island fasciocutaneous flap based on a single dissected perforator, which reaches the recipient site through an axial rotation. [9, 10] The main advantages of any local flap and also of the pedicle perforator flaps are represented by the one stage operation with the possibility to cover the defect with like to like tissues, minimal donor-site morbidity, shorter surgery duration, and reduce hospitalization time. [16-19]
The most important principles that need to be fulfilled for the use of pedicle perforator flaps are: a good condition of surrounding tissues, the dimension of the defect which must be covered with the flap, and the presence of perforator pedicle in the proximity of the defect with a good flow of the artery to support the rotation. [16]
The risks are minimized if a proper selection of the patient and a careful dissection of the perforator pedicle are made. Any conditions, such as local trauma, prolonged edema, history of irradiation, perilesional scars or arteriopathy, are important and should be considered when choosing a perforating flap. [16, 17, 20, 21] Our patient was young - 40 years old, without any medical history, not smoking, and with an athletic constitution.
Regarding the size of the perforator flap, there is no significant data in the literature to point a safe dimension which can be harvested. The perforasome theory explains how ligations of adjacent perforators increase the blood flow in the pedicle and the supplied skin territory, but the exact flap dimension is difficult to appreciate. [22] Teo described flaps up to 210cm2, D’Arpa in his study on 85 Consecutive Cases had flaps with length ranged from 7 to 26 cm and the width from 4 to 6 cm. [9, 23] The maximum size flap found by Yasir et al. in their study that was 190 cm2 raised on a single perforator for the knee coverage. [24] In our case the flap was a large one - 25/7 cm (175cm2) because a subsequent Achilles tendon and calcaneus reconstruction was taken into consideration.
The localization of the perforator is usually done with a hand-held Doppler; more elaborate explorations like angiography or angioscanner are useful, but not absolutely necessary. The proximity of a perforator with a good blood flow is a very important criterion when planning a propeller flap. Adam Stepniewski et al., and also Brunetti et al. recommended that the distance between the perforator and the defect should not exceed the length of the defect diameter for a propeller flap. [16, 25] This position will determine the pivot point of the flap and the size of the flap. The pedicle has to support variable angle of the torsional twist, up to 180 degrees. [9] Wong in his paper about perforator patency in propeller flaps recommended that the pedicle has to be 1 mm in diameter and more than 30 mm in length. [26] Still, the correlation between size of perforator, the blood flow through it and the size of flap that can be safely risen is not found yet.
Regarding the general risk factors for complication of pedicle perforator flaps in the distal third of leg, Gir et al. in his review of 15 publications found no significant differences related to age, gender, etiology or location of the defect, type or size of the flap. [27] Later, Bekara et al. in their meta-analysis identified three significant risk factors: age older than 60 years, diabetes, and arteriopathy. [21]
Compared with the free flap, Rodriguez-Collazo E et al. in their review found no significant differences in flap selection based on reliability of flap outcomes. An ideal flap transfer for reconstruction of lower extremity soft tissue defects has not yet been established, both methods having advantages and disadvantages. [16, 28] For pedicle perforator flaps, disadvantages are related to the application for small to midsize defects, and to the necessity of the presence of perforators close to the defect. [28]
Conclusions
We found propeller flaps to be a reliable tool for lower-extremity reconstruction, especially considering that any reconstruction should start from a simpler method to a more complex one. If a proper selection of the patient is made, the perforator pedicle flaps are a viable option to the free flaps, with low complication rate, and a more functional and aesthetical result.
References
